Alberta Health administers AAHB; however, Community and Social Services process enrolment in the program. AAHB is intended as a support to Albertans in low income to ensure they have access to prescription drugs, dental services, optical services, emergency ambulance and diabetic supplies that are essential to health and well-being.
The AAHB program is provided as an extension of health benefits offered through the Community and Income Support and AISH programs, to assist eligible persons leaving the programs to maintain employment.
The AAHB is also available to women during pregnancy and to households with high ongoing prescription drug needs, if their household incomes are within the AAHB qualifying income levels.
AAHB is a means-tested benefit. Eligible applicants may be: pregnant; have high ongoing prescription drug needs; refugee or refugee claimants not otherwise receiving health benefits from any other source; or leaving the Income Support or AISH programs due to excess income. People who would ordinarily not qualify for AAHB based on income, but have high drugs needs may qualify (total annual income – annual drug cost = adjusted income). If you have dependant children under the age of 18 and are low-income, see: Alberta Child Health Benefit for information.
Please note: Eligible applicants must have an annual household I not above qualifying levels. You must have completed your income tax return for the most recent year before applying. If your current annual income is lower than your last reported annual income, contact the Health Benefits Contact Centre.
To apply for AAHB, complete an application, and submit to Health Benefits Contact Centre by fax or mail. For assistance in completing your application, have your physician refer you to a social worker, or contact Alberta Supports.
Important Links
AAHB (All Information)
AAHB Application
AAHB (What’s Covered)
The Alberta Child Health Benefit (ACHB) covers children’s health expenses for families with low incomes. This health plan is for children up to 18 years of age. Children who are 18 or 19 years old also qualify, if they are living at home and attending high school. ACHB is a means-tested benefit. The total combined household net income plus non- taxable child support income received must be equal to or less than the applicable qualifying income level.
Please note: To be eligible for the ACHB, you and members of your family must be a low-income resident of Alberta, with an annual income below current threshold levels. You must have a Notice of Assessment (NOA) for the most current tax year in order to apply. If your current annual income is lower than your NOA, contact the Health Benefits Contact Centre for an exception.
To apply for ACHB, complete an application, and submit to Health Benefits Contact Centre by fax or mail. For assistance in completing your application, have your physician refer you to a social worker, or contact Alberta Supports.
Important Links
ACHB (All Information)
ACHB Eligibility
ACHB Application
AISH and Income Support (BFE and ETW subtypes) are eligible to receive similar health benefit coverage provided for by the Alberta Adult Health Benefit (AAHB) and Alberta Child Health Benefit (ACHB) programs. People applying for AISH and Income Support will receive a health benefits card automatically upon the approval of their application.
Recipients of One-Time (Emergency) benefits through Income Support are able to access funds for up to one month of prescription medication, along with other emergency expenses.
Call the 24-hour Emergency Income Support Contact Centre (available 24/7):
Toll free: 1-866-644-5135 TTY toll free: 1-800-232-7215 (ask to speak to Alberta Supports) Fax: 780-422-9681 Email: [email protected] (responses may take 1-3 business days)
Give your pharmacy fax number and contact information to the Alberta Works worker you speak to. The worker will provide your pharmacist with a code valid for 24 hours in order for your prescription to be covered under emergency benefits.
The Non-Group Coverage program ensures all Albertans have access to an economical supplementary health benefits program. The program provides coverage for a variety of health-related services not covered by the Alberta Health Care Insurance Plan (AHCIP).
Alberta Blue Cross administers Non-Group Coverage on behalf of the Alberta government.
A monthly premium is charged for Non-Group Coverage. If your household income is too high to qualify for AAHB/ACHB, but falls under this threshold, you may be eligible to receive a subsidized premium for Non-Group Coverage.
Please note: This program does not provide travel coverage. If you are planning to travel outside of the province or country, you should purchase travel insurance to cover emergency hospital and medical expenses.
A $50 annual deductible is applied to the total of all eligible health benefit expenses incurred in a benefit year, except for prescription drugs and diabetic supplies. The benefit year runs from July 1 to June 30. When no claim has been made for health benefits in a benefit year, any such expenses incurred during April, May or June that do not exceed $50 may be carried forward into the next benefit year and credited, in whole or in part, toward the deductible in that year.
For prescription drugs, the co-payment is 30% to a maximum of $25. A co-payment is the portion of the prescription cost you pay to your pharmacy when you have your prescription filled. For most prescriptions, you will not pay more than $25 for each prescription. Prescription drugs covered under the plan are listed in the Alberta Drug Benefit List.
Benefits include diabetic supplies, ambulance services, clinical psychological services, home nursing care, prosthetic and orthotic benefits, mastectomy prosthesis, and hospital accommodation (semi-private).
These benefits include an annual maximum, and are subject to a $50 annual deductible (total per annum). Prescription medications are not subject to this deductible (see above).
Important Links
Non-Group Coverage (All Information)
Eligibility for Monthly Premium Subsidy
Non-Group Coverage Application
Seniors, their spouses/interdependent partners and dependants registered on the same Alberta Health Care Insurance Plan (AHCIP) account receive a premium-free benefit to provide coverage for prescriptions and other health-related services not covered under the AHCIP.
Alberta Blue Cross administers the Coverage for Seniors program and claims. AHCIP manages eligibility and registration.
Please note: This program does not provide travel coverage. If you are planning to travel outside of the province or country, you should purchase travel insurance to cover emergency hospital and medical expenses.
To be eligible for Coverage for Seniors, you must provide proof of being 65 years of age or older. When AHCIP records indicate an Albertan will be turning 65, a package is mailed to the address on their AHCIP file providing information about programs and services for seniors. This package will include a letter asking you to submit proof-of-age documents if required. If you did not receive the package, or have further questions, contact the AHCIP office.
If AHCIP have a proof-of-age document on your AHCIP file, Coverage for Seniors is automatically added to your AHCIP account. If you are unsure if you are already covered, call Health Link (811) with your AHCIP number ready to inquire.
If AHCIP does not have a proof-of-age document on your AHCIP file, you will need to submit a proof-of-age document and a completed Proof-of-Age Declaration form.
Acceptable proof-of-age documents include: birth certificate, old-age pension entitlement form, passport or immigration record, or Canadian citizenship certificate.
Take your proof-of-age document and declaration to an AHCIP authorized registry agent for processing. You can also mail the completed form and a copy (both sides) of the proof-of-age document to the AHCIP office.
Low-income seniors may qualify for additional funding for medical supplies and equipment through SNA-Seniors, including a portion of prescription drug co-payments.
Important Links
Coverage for Seniors (All Information)
Coverage for Seniors Benefit Information
The Palliative Coverage Program provides subsidized benefits to Albertans who are diagnosed as palliative and remain in their home or in a hospice where access to publicly funded drugs, diabetic supplies, and ambulance services are not included.
Albertans who are palliative are provided access to supplementary health benefits that provide coverage for health-related services not covered by the Alberta Health Care Insurance Plan (AHCIP) through this program.
Alberta Blue Cross administers the Palliative Coverage program. There are no premiums to pay. The program is open to Albertans registered with the AHCIP and who have been diagnosed as being palliative.
Palliative refers to patients who have been diagnosed by a physician or nurse practitioner as being in the end stage of a terminal illness or disease. Patients are aware of their diagnosis and have made a voluntary informed decision related to resuscitation, and the focus of care is palliation and not treatment aimed at a cure.
Please note: The program excludes patients who live in residences that provide publicly funded drugs, diabetic supplies and ambulance service, including long-term care facilities, acute care hospitals, and psychiatric hospitals.
To apply for the Palliative Coverage Program, download and complete the application form. The application form must be completed and signed by both the affected patient, or guardian, and physician or nurse practitioner.
The patient or guardian will receive written notification from the Ministry of Health regarding acceptance into the program. Alberta Blue Cross will mail an ID card to the patient or guardian.
The physician or nurse practitioner determines the effective date of coverage. This date must not be more than 30 days prior to the date the program office receives the application. The coverage will continue if the patient is diagnosed as being palliative.
This program covers prescription medications, specific laxatives and solutions for hydration therapy are covered if listed in the Alberta Drug Benefit List or Palliative Care Drug Benefit Supplement. You will be responsible for 30% of the cost of the prescription to a maximum of $25 co-payment, and a lifetime maximum of $1,000.
Please note: You may be responsible for additional costs if: your drug is not listed in the Alberta Drug Benefit List; or you want a more expensive brand of drug than the lowest- cost option, maximum allowable cost product, or generic product; or the brand of drug you want costs more than the maximum amount set by the Alberta government for that drug.
Important Links
Palliative Coverage (All Information)
Palliative Coverage Application
How to Claim Benefits though Alberta Blue Cross
The Non-Insured Health Benefits (NIHB) Program of the Department of Indigenous Services Canada provides eligible clients (persons with registered First Nations status and recognized Inuit) with coverage for a range of health benefits, including prescription drugs and over-the-counter medications, dental and vision care, medical supplies and equipment, mental health counselling, and transportation to access health services not available locally.
These benefits complement ACHIP coverage, which includes physician and hospital care, as well as other First Nations-oriented community programs and services. For low-income Albertans with First Nations status, you can access benefits not covered by NIHB through different provincial benefit programs (i.e. AISH, Income Support, AAHB). If you experience difficulty obtaining coverage due to the coordination of these benefits, ask a social worker to assist you.
Benefits include drugs, medical transportation, dental care, medical supplies and equipment, crisis intervention counselling and vision care.
If you require assistance with accessing benefits, have inquiries about coverage, or any other questions, contact your band worker or have a social worker assist you in contacting NIHB.
Important Links
NIHB Contact Information
NIHB Client Reimbursement Form
NIHB Eligibility
NIHB Guides

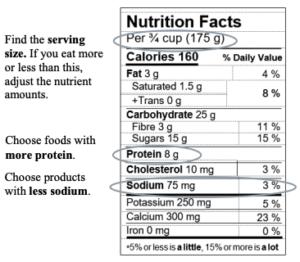
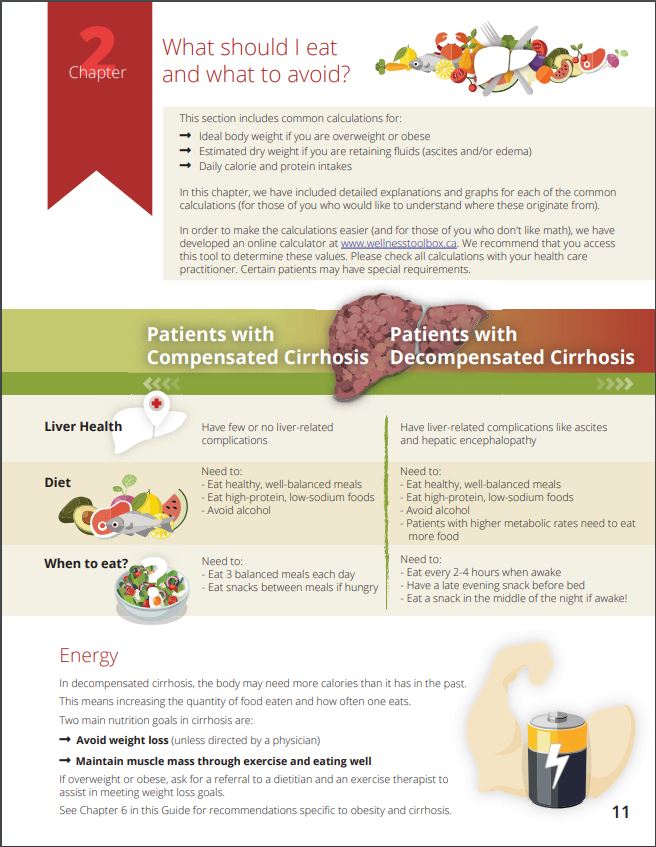
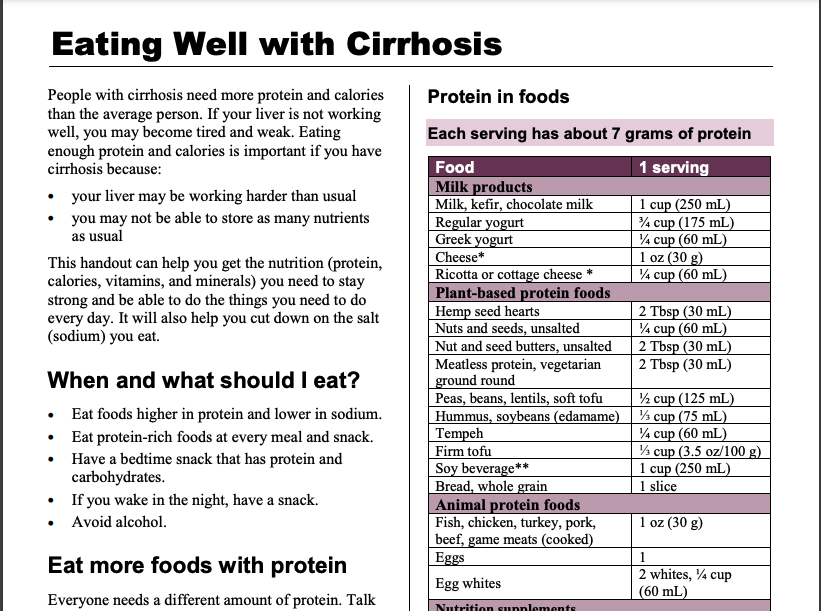
 Our national team of healthcare practitioners specializing in cirrhosis developed a practical “nutrition tool”
Our national team of healthcare practitioners specializing in cirrhosis developed a practical “nutrition tool”