When to get Help
Only mild symptoms of confusion (hepatic encephalopathy) should be managed at home.
Go to the nearest emergency department, or have someone call 911 if you:
- have severe confusion or sleepiness
- can’t speak, walk properly, or follow directions
- have a fever
- have severe nausea and vomiting
What is Hepatic Encephalopathy?
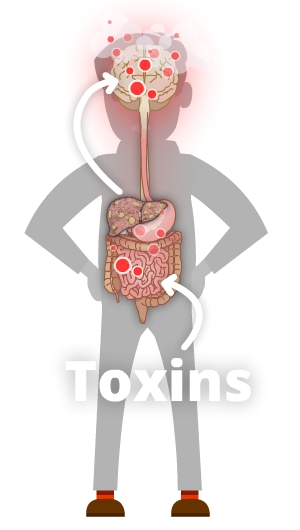
When the liver’s been damaged by cirrhosis, it might not be able to get rid of toxins such as ammonia. As a result, ammonia and other toxins may build up in your bloodstream and brain. This causes a problem called hepatic encephalopathy (pronounced “en-sef-a-lop-a-thee”). You may hear your healthcare team call it HE for short. When you have HE, toxins build up which can cause confusion and other symptoms.
Causes
Encephalopathy is most likely to occur in people who have high pressure in their portal vein (portal hypertension). It may also occur in people who have severe acute liver damage (liver damage that happens suddenly) but no portal hypertension.
Also, a procedure called TIPS that is used to lower portal hypertension by shunting blood flow around the liver can increase your risk for encephalopathy.
Other things that might contribute to encephalopathy include:
- abnormal levels of electrolytes
- constipation
- not getting enough fluids to drink or loosing fluids too quickly (dehydration)
- internal bleeding
- infection
- medicines like pain killers and sleeping pills
Symptoms
Symptoms of encephalopathy might include:
- coma
- disorientation (not remembering where you are or what’s happening)
- difficulty remembering the right words to say
- drowsiness
- hand “flapping”
- sleep pattern changes
- feeling irritable
- trouble concentrating
- poor short-term memory
- having tremors
Treatment
Your Support Network
Share what you learn about hepatic encephalopathy with your caregivers, friends, and loved ones. This is important because having encephalopathy can make it hard for you to care for yourself at times, and you may need extra support. Your support network can help you watch for emergency warning signs. For example, if they notice you’re really confused or have trouble waking up, they can call 911 or take you to the nearest emergency department.
Lactulose
In most situations, encephalopathy is treated with a medicine called lactulose. Lactulose is a laxative syrup that makes your bowels move more often and also makes your bowel movements more acidic. This helps your body to get rid of toxins like ammonia from your body.
If you are taking lactulose, you should take enough so that you are having 2 or 3 soft bowel movements each day. If you take too much you will get diarrhea, but if you don’t take enough you will develop encephalopathy symptoms. You should increase the amount you are taking if you are not having enough bowel movements. Finding the right balance for you is the key. You can get more information about lactulose (including potential side effects) from your pharmacist.

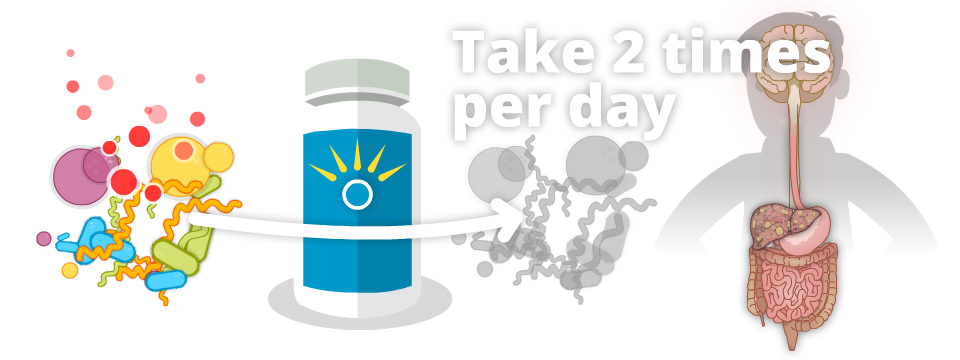
Rifaximin (Zaxine, Xifaxan)
Another treatment for encephalopathy is rifaximin. Rifaximin is an antibiotic that stays in your digestive system and changes the bacteria in your gut so they make less toxins like ammonia. Rifaximin comes as a pill and is usually taken two times a day. You can take it with or without food. You can get more information about rifaximin (including potential side effects) from your pharmacist.
Self Care Tips:
If you are being treated for hepatic encephalopathy:
- Avoid medicines that can make you sleepy
- Record the number of bowel movements you have each day in a notebook or app on your phone
- Take enough lactulose so you have 2 to 3 medium to large, soft bowel movements a day.
- Don’t take more lactulose than you need because it may make you dehydrated.
- If you develop a mild increase in your encephalopathy symptoms, take more lactulose (as long as you are not having diarrhea, fever, or signs of bleeding).
Let your healthcare provider know if you:
- have trouble adjusting your dose of lactulose
- feel tired, sleep more, or your sleep patterns change so you’re up at night and sleep during the day
- have trouble concentrating or remembering things
- have a change in your personality
- notice shaking of your body (called a tremor) or are unsteady (feel like you may fall)
References:
The information on this page was adapted (with permission) from the references below, by the Cirrhosis Care Alberta project team (physicians, nurse practitioners, registered nurses, registered dietitians, physiotherapists, pharmacists, and patient advisors).
This information is not intended to replace advice from your healthcare team. They know your medical situation best. Always follow your healthcare team’s advice.
References:

