Embolization is performed in the hospital, usually by a specially trained doctor called an Interventional Radiologist. Depending on the type of embolization procedure you have, you may need to stay overnight in the hospital, or you might be able to go home the same day.
The Procedure:
Before the procedure begins, you will have an intravenous placed to give you medications. In the procedure room, you will lay on the procedure table and a nurse will set up monitors to measure your blood pressure, heart rate and oxygen levels. The doctor will go over the procedure and its potential risks and benefits.
The procedure will begin with you receiving sedation through your intravenous to make you more relaxed. You may also be given antibiotics. In some cases you may be given general anesthesia. The doctor will then make a small cut in your upper leg. Through this cut, a thin flexible tube (called a catheter) will be placed inside a blood vessel in your leg. In some cases, this catheter might be inserted through a blood vessel in your wrist instead.
The doctor will guide the catheter through the blood vessel… until it reaches your liver…and then guide it to the tumor. Special scans will be used during the procedure to see where the catheter is at all times.
Once the catheter reaches the tumor, particles will be injected through the catheter to block blood flow and shrink the tumor.
There are 3 different types of embolization:
- Bland Embolization: During Bland embolization bland particles are injected into the tumor to block off it’s blood
- Transarterial Chemoembolization (TACE): the particles injected through the catheter block off the blood supply and also contain chemotherapy medication that helps destroy the tumor.
- Transarterial Radioembolization (TARE): the particles supplied to the site of the tumor contain radioactive material that helps to destroy the tumor. If you are booked for a TARE procedure, you may need to come in for a simulation appointment a few days before the treatment so the healthcare team can take pictures of your liver and give you test doses to plan for the actual procedure.
Pain, fever and nausea can happen with the embolization procedures, but medications can be given to manage these symptoms. No matter which type of embolization procedure you have, it will usually take 1 to 2 hours. After the embolization is complete, the catheter is removed and a dressing is placed over the area the cut was made. In most cases, you will be asked to rest and lie flat for up to 6 hours.
After the Procedure:
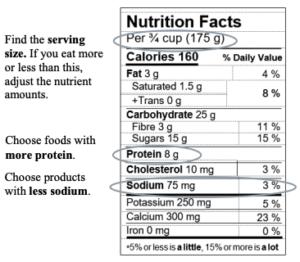
For the first 10 days after your embolization, you should take it easy, drink lots of water, and avoid strenuous activities or lifting more than 5lbs. Each person’s recovery experience will be different. Some people may feel tired for up to 3 weeks after the embolization. If you develop fever or chills, sudden or worsening pain, trouble eating or drinking because of nausea and vomiting, bleeding or swelling at the site where the cut was made, or any other new or concerning symptoms, please contact your doctor or nurse right away.
Your healthcare team will arrange a follow-up scan (like ultrasound, MRI or CT) which will involve taking pictures of the liver and using a special contrast dye to help make the tumor area more visible. This is usually done about 1-3 months after the embolization. Based on the results of your scan, your healthcare team will decide if any more treatment for your HCC is recommended and when more scans should be done. Scans are usually done more often in the first 2 years after treatment.
You should also continue to monitor yourself for development of any new symptoms and have blood work checked as recommended so your health care team can monitor your liver.
Embolization procedures are not usually considered curative, meaning they do not cure liver cancer. Instead, they are used to shrink HCC tumors or slow down their growth. Depending on the type of embolization you have, how well it works, how many tumors you have, and your liver function, more HCC procedures may be recommended for you in the future.
References:
The information on this page was adapted (with permission) from the references below, by the Cirrhosis Care Alberta project team (physicians, nurse practitioners, registered nurses, registered dietitians, physiotherapists, pharmacists, and patient advisors).
This information is not intended to replace advice from your healthcare team. They know your medical situation best. Always follow your healthcare team’s advice.
References: