Top tips:
-
- Validated assessment tools should be used to assess for delirium
- Hepatic encephalopathy is a major contributor to delirium/agitation and must be considered as the diagnosis of exclusion in any patient presenting with confusion.
- Before using this algorithm, it is essential to distinguish these two patients*:
- Advanced cirrhosis not at the end of life where confusion may be due to Hepatic encephalopathy – confusion CAN recover with Hepatic encephalopathy therapy, (see Hepatic encephalopathy page). Some of these patients may still be candidates for liver transplantation if it is in keeping with their goals of care. Hepatic encephalopathy MUST be ruled out before using this algorithm.
- Advanced cirrhosis at the end of life (last weeks to days) with delirium/agitation who are not candidates for liver transplantation and do not want further management for their Hepatic encephalopathy. Can use the algorithm.
*This distinction can be challenging. A trial of lactulose can be helpful. Ask for advice from a liver specialist if guidance is required.
- In addition to Hepatic Encephalopathy, consider additional workup to identify and manage reversible causes of delirium
- Even at end-of-life, if it is in keeping with the patient’s goals of care, therapy with lactulose and/or rifaximin can be continued while the patient is able to swallow.

Use validated tools to define delirium vs. agitation and restlessness (e.g. Confusion Assessment Method, CAM)
Consider contributing causes for delirium and investigate & treat if in keeping with the patient’s goals of care.
Hepatic Encephalopathy (HE) is the diagnosis of exclusion in these patients, especially in those with a prior history of HE (see the HE page link for more information).
**Unless there is an obvious non-HE precipitant, provide a trial of lactulose therapy BEFORE moving any further in the algorithm.
- D: Drugs/toxins – Drug/alcohol intoxication or withdrawal. Renal and/or liver dysfunction may increase the risk of drug or toxin accumulation; opioid toxicity can be a contributing factor – rotate opioids and hydrate if this is suspected
- I: Infection – primary peritoneal, urologic or alternate site
- M: Metabolic – hepatic encephalopathy, electrolyte abnormalities, thyroid dysfunction, CO2, O2 abnormalities
- S: Structural – primary CNS – tumour, hemorrhage, edema, seizure, underlying dementia
- O: Other – psychiatric disease, shock/intravascular, neoplastic, withdrawal, deficiencies, inflammatory/autoimm
Consider Non-pharmacological therapy in addition to PRN pharmacological therapies in patients where delirium and associated symptoms (restlessness, agitation, perceptual disturbances – hallucinations, delusions) are having a significant impact on the patient’s quality of life and ability to function.
- Interactions with and involvement of family
- Orientation with calendars/clocks/photos
- Ensuring adequate hydration
- Ensuring that the patient has glasses and hearing aids if needed,
- Maintaining sleep-wake cycle
- Pain: Delirium may mask a patient’s ability to express symptom burden of pain. This is especially true in agitated delirium and pain assessment may be difficult. Ensure any symptoms of pain are adequately managed.
- Alterations in other bodily functions such as urination (e.g. urinary retention) and defecation (e.g. severe constipation) may be more challenging to assess and may also contribute to restlessness and agitation.
Always consider degree of sedation when selecting a medication. It is critical to assess the patient’s preference/tolerance of sleepiness, especially if regular doses are required.
There are only a few instances where benzodiazepines, e.g. lorazepam, should be the first choice as an alternative to or alongside the below mentioned neuroleptic medications
- Alcohol withdrawal (see CCAB Alcoholic hepatitis page)
- Benzodiazepine withdrawal
- Long-term benzodiazepine use
- Start at the lowest dose and titrate (unless symptoms are severe and drowsiness is part of expected goals)
- More sedating medications can be used for admitted patients
- Only use one neuroleptic at one time
- Monitor for Extrapyramidal symptoms (EPS) in all patients taking neuroleptic medications
| Medication: | Recommended Dose | Additional information |
|---|---|---|
|
Haloperidol |
0.5 mg- 1 mg PO/SC q1h PRN
|
|
|
Quetiapine |
10 mg PO TID |
|
|
Olanzapine |
2.5 mg PO q4h PRN |
|
- If patient is requiring several doses of PRN medications, consider increasing Neuroleptic medications to ATC (around the clock) dosing.
- Typically dosed q4h, but frequently can be modified depending on severity (eg q12 hr to start)
- Aim for the lowest effective dose to minimize adverse effects and sedation
- Only use ONE neuroleptic at a time- stop the previous medication when starting another one
- Start with Haloperidol. If it is ineffective, then titrate in order from least to most sedating.
- Monitor for Extrapyramidal symptoms (EPS) in all patients taking neuroleptic medications
- Continue to routinely review medical status with substitute decision-makers. Worsening agitation may indicate irreversible delirium and short prognosis
| Medication: | Recommended Dose | Additional information |
|---|---|---|
|
Haloperidol |
0.5 mg -1 mg PO/SC q 8h ATC AND
|
|
|
Quetiapine |
6.25 mg-12.5 mg PO q4h PRN |
|
|
Olanzapine |
2.5 mg PO q4h PRN |
|
If symptoms persist despite the management above, review medical status and goals of care.
Stop Haloperidol or other Neuroleptic
| Medication: | Recommended Dose | Additional information |
|---|---|---|
|
Methotrimeprazine (Nozinan) |
6.5 mg-12.5 mg PO/SC q8 h ATC AND q 1h PRN
|
-Least risk of seizures. |
- Re-evaluate prognosis and discuss with patient/agent.
- If focus shifts to comfort only and end of life, Palliative sedation (e.g. Continuous Midazolam infusion) might be indicated now. Palliative consultation is highly recommended for this. See AHS guidelines for palliative sedation.
We gratefully acknowledge the Physician Learning Program for their design assistance.
This section was adapted from content using the following evidence based resources in combination with expert consensus. The presented information is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient’s care.
Authors (Alphabetical): Amanda Brisebois, Sarah Burton-Macleod, Ingrid DeKock , Martin Labrie, Noush Mirhosseini, Mino Mitri, Kinjal Patel, Aynharan Sinnarajah, Puneeta Tandon
Thank you to pharmacists Omer Ghutmy and Meghan Mior for their help with reviewing these pages.
Helpful Links:
- Confusion Assessment Method (CAM):
https://www.albertahealthservices.ca/assets/about/scn/ahs-scn-bjh-hf-delirium-screening-tool.pdf - Hepatic Encephalopathy:
http://cirrhosiscare.ca/treatment-provider/hepatic-encephalopathy-hcp/
- Opioid Toxicity:
https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-peolc-provincial-guideline-for-treatment-opioid-neurotoxicity.pdf
References:
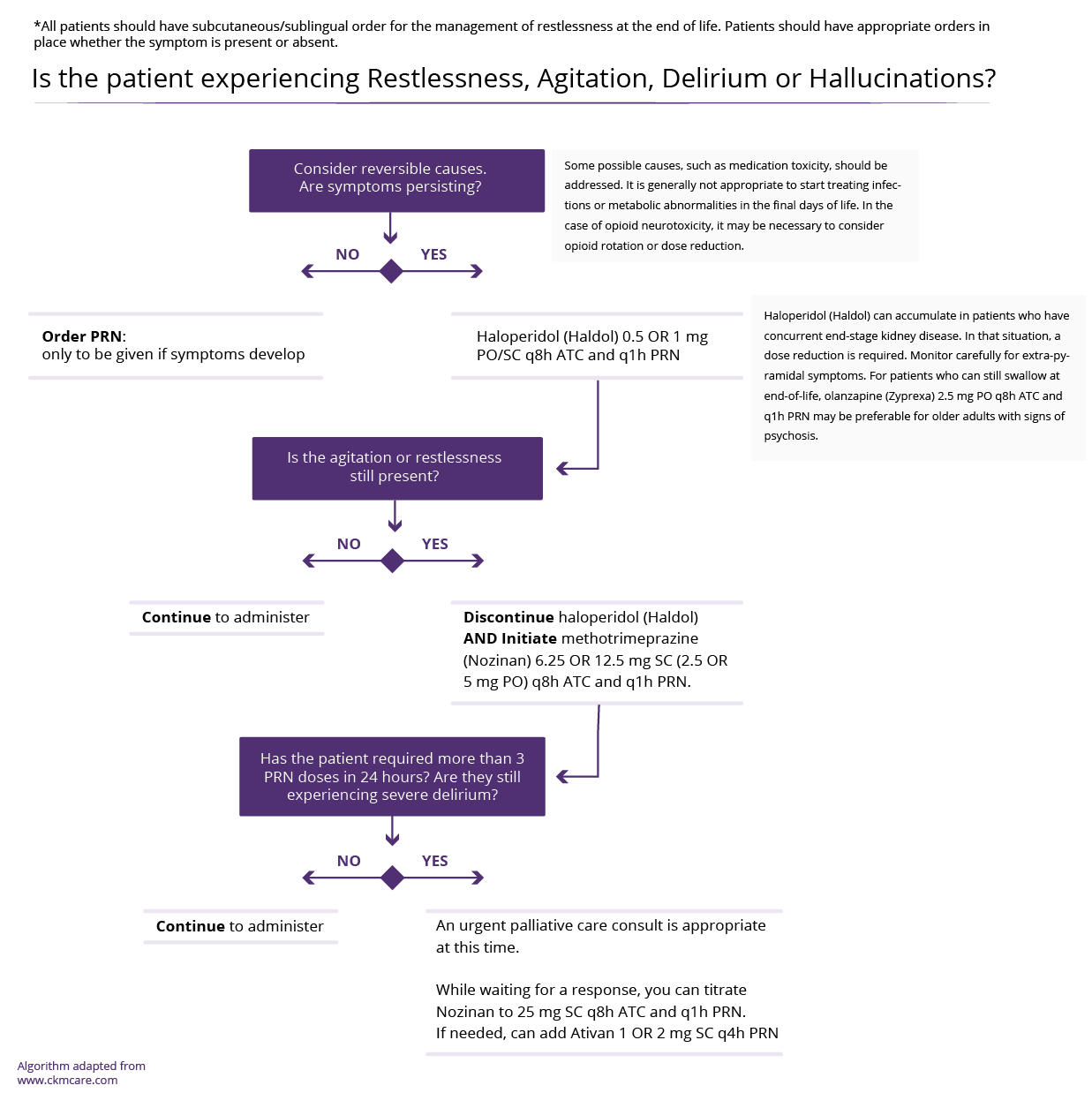
- Davison SN on behalf of the Kidney Supportive Care Research Group. Conservative Kidney Management Pathway; Available from: https//:www.CKMcare.com.
- Palliative sedation guidelines: http://www.cspcp.ca/wp-content/uploads/2017/11/Palliative-Sedation-Edmonton-Final-Dec-2015.pdf
- Palliative care tips/delirium in patients with advanced cancer and those who are imminently dying: https://albertahealthservices.ca/info/Page16872.aspx
- Agar, M. et. al. Efficacy of Oral Risperidone, Haloperidol, or Placebo for Symptoms of Delirium Among Patients in Palliative Care: A Randomized Clinical Trial. JAMA Internal Medicine 177(1): 34-42. PMID: 27918778
- Bush, SH., Tierney, S., and Lawlor, PG. Clinical Assessment and Management of Delirium in the Palliative Care Setting. 2017. Drugs 77:1623-1643. PMID: 28864877
- Bush, SH., et. al. Treating an Established Episode of Delirium in Palliative Care: Expert Opinion and Review of the Current Evidence Base with Recommendations for Future Development. 2014. JPSM 48(2): 231-248. PMID: 24480529
- De la Cruz, M., et. al. Increased Symptom expression among Patients with Delirium Admitted to an Acute Palliative Care Unit. 2017. Journal of Palliative Medicine. 20(6): 638-641. PMID: 28157431
- Hui, D. Benzodiazepines for agitation in patients with delirium: selecting the right patient, right time, and right indication. 2018.Curr Opin Support Palliat Care 12: 489-494. PMID: 30239384
- Hui, D. et. al. Effect of Lorazepam with Haloperidol vs Haloperidol alone on Agitated Delirium in Patients With advanced Cancer Receiving Palliative Care: A Randomized Clinical Trial. 2017. JAMA. 318(11): 1047-1056. PMID: 28975307
- Lewis J. H., Stine J. G. Review article: prescribing medications in patients with cirrhosis – a practical guide. Aliment Pharmacol Ther 2013; 37: 1132–1156. PMID: 23638982
- Oh, E. et. al. Delirium in Older Persons: Advances in Diagnosis and Treatment. 2017. JAMA 318(12): 1161-1174. PMID: 28973626